Aside from information about the affected U.S. states experiencing an E. coli outbreak, the CDC has also shared a list of food brands that have been recalled and prevention tips.
On November 17, the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA) alerted the public that there is a new E. coli outbreak in the U.S. that is linked to organic carrots. They have revealed which products have been recalled, the affected states, case statistics, symptoms, and what people should do to avoid infection.
The CDC and FDC confirmed that the E. coli outbreak is linked to organic whole and baby carrots of multiple sizes distributed by Grimmway Farms.
Although the supplier company issued a recall of the implicated products on November 16, the CDC warns that some of the recalled bagged carrots may still be present in consumers’ homes, even if they are no longer available on the shelves of local supermarkets.
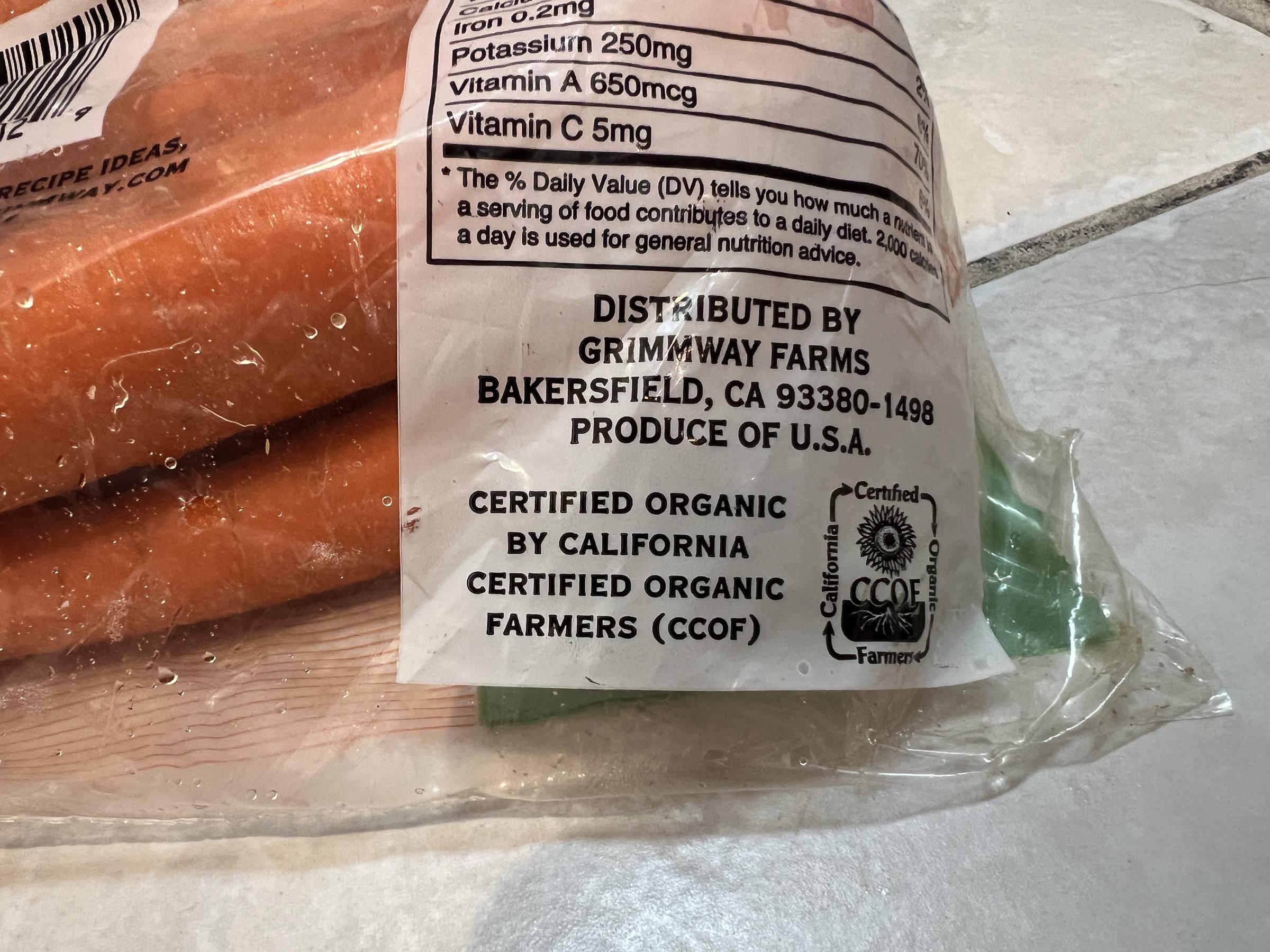
A close-up photo of a Grimmway Farms information label in Lafayette, California on November 17, 2024 | Source: Getty Images
People are advised to check their refrigerators for any brands of organic whole or baby carrots that have been recalled, and immediately discard or return them to the store.
Businesses are also cautioned against selling such items and have been urged to wash and sanitize any surfaces or objects that may have come into contact with the recalled carrots.

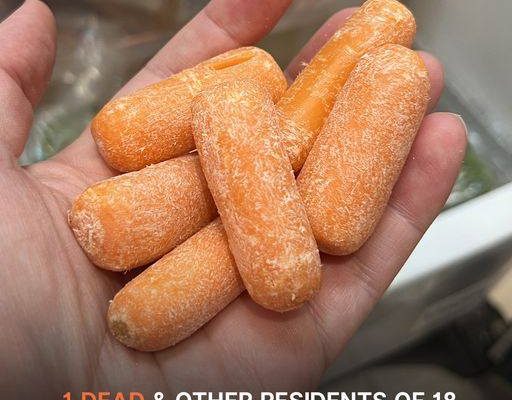
An individual holding a bunch of baby carrots from their fridge in Lafayette, California. | Source: Getty
Grimmway Farms’ product recall consists of a comprehensive list of several brands. The affected brands include well-known names such as 365, Bunny Luv, Cal-Organic, Compliments, Full Circle, Good & Gather, GreenWise, and Marketside.

A close-up photo of a packet of Bunny Luv organic carrots from Grimmway Farms in Lafayette, California. | Source: Getty Images
Others include Nature’s Promise, O-Organic, President’s Choice, Raley’s, Simple Truth, Sprouts, Trader Joe’s, Wegmans, and Wholesome Pantry. The recalled baby organic carrots feature best-if-used-by dates ranging from September 11 to November 12.
Although the whole organic carrots have no specific best-if-used-by dates listed on the bags, these products were available for purchase in stores between August 14 and October 23. Whole organic carrot brands that are affected by the E.coli product recall are identical to the ones for the baby carrots.
The E. coli outbreak has been confirmed in 18 states across the U.S., with a total of 39 reported illnesses, 15 hospitalizations, and one death. Additionally, the last reported illness onset occurred on October 28.
Affected states include Arkansas, California, Colorado, Massachusetts, Michigan, Minnesota, Missouri, North Carolina, New Jersey, New York, Ohio, Oregon, Pennsylvania, South Carolina, Texas, Virginia, Washington, and Wyoming.
Interviews conducted with 27 individuals who fell ill revealed that 26 (96%) had consumed carrots in the week prior to experiencing symptoms, solidifying the link to the recalled products.
According to a case count map provided by the CDC, states like Minnesota, New York, and Washington are experiencing higher concentrations of cases, with other states such as Wyoming, California, and Texas showing a more scattered spread.
The recalled organic carrots were contaminated with Shiga toxin-producing Escherichia coli (E. coli) O121:H19, which is a dangerous strain of bacteria known to cause severe and sometimes life-threatening infections.
This strain poses a heightened risk to young children, the elderly, and individuals with compromised immune systems.
In severe cases, infections may lead to complications such as kidney issues (hemolytic uremic syndrome a.k.a HUS). This is a condition that can cause kidney failure, and in some severe cases, death. Common symptoms of an E. coli infection, which typically appear three to four days after exposure, include intense stomach cramps, diarrhea (often bloody) fever, nausea, and vomiting.
Usually, most people recover after five to seven days without needing treatment. However, some people require hospitalization if they develop serious kidney problems. The CDC urges anyone experiencing severe symptoms like signs of dehydration, continuous diarrhea, and a fever higher than 102°F to seek medical care.
Escherichia coli, commonly known as E. coli, are bacteria that exist in a variety of environments, including food, water, and the intestines of people and animals.
While most strains of E. coli are harmless and play a vital role in a healthy intestinal system, helping to digest food, produce vitamins, and combat harmful germs, certain strains can cause severe illness.
Infection often occurs when individuals consume E. coli through contaminated food or water, or direct contact with infected animals, people, or environments.
Vulnerable populations, including adults aged 65 and older and international travelers, are at higher risk of infection.
To minimize the risk of contracting E. coli, the CDC has shared an array of prevention tips that focus on proper food handling, cleanliness, and vigilance with water and beverages.
Frequent handwashing remains one of the most effective ways to reduce the spread of harmful bacteria. Civilians should wash their hands for at least 20 seconds with soap and water before, during, and after food preparation, and always after handling raw ingredients like meat, poultry, or eggs.
Kitchen surfaces, utensils, and cutting boards should also be washed thoroughly with hot, soapy water between uses to prevent cross-contamination. Additionally, fresh fruits and vegetables should be rinsed under running water before consumption.
Keeping raw meat, poultry, seafood, and eggs separate from other foods is also crucial. People should use different cutting boards for raw and ready-to-eat items, and store raw foods in sealed containers to prevent juices from leaking. Notably, the CDC advises against washing raw chicken as it can spread bacteria to kitchen surfaces.
When it comes to cooking food, finding the correct internal temperature is vital for killing harmful bacteria like E. coli. One should also use a food thermometer to ensure accuracy.
The CDC recommends specific temperatures such as 145°F for whole cuts of meat, 160°F for ground meats, and 165°F for poultry and leftovers.
Additionally, people should refrigerate perishable foods promptly (within two hours, or one hour if temperatures exceed 90°F) and keep their refrigerators at 40°F or below to inhibit bacterial growth.
Other prevention measures involve ensuring access to safe drinking water. When camping, hiking, or traveling, people should ensure water is treated to avoid contamination.
Similarly, one should avoid swallowing water while swimming in lakes, ponds, or pools, and never swim if experiencing diarrhea.
Lastly, civilians should only consume milk, juices, and dairy products that are clearly labeled as pasteurized. This process kills harmful germs, including E. coli, and ensures a safer food and beverage experience.
By following these steps, individuals can greatly reduce their risk of E. coli infection and other foodborne illnesses, ensuring the protection of themselves and their loved ones.